Abstract
This article summarizes key characteristics of a successful private practice group in Infectious Disease based on the experience of Metro Infectious Disease Consultants.
Introduction
Success in clinical practice can be defined by various attributes, including personal fulfillment, work–life balance, financial viability, mental stimulation and challenge, and the camaraderie and support of a thriving group. Infectious disease (ID) physicians often find personal satisfaction in treating underprivileged patients, the mental stimulation of working on intriguing cases, and the fellowship of peers. These are some of the characteristics that draw residents into the field of ID.
The inability to achieve financial success has been a common reason for dissatisfaction among ID physicians over the past several years. Fewer qualified residents have been entering the ID workforce, as evidenced by an increase in the number of vacant fellowship positions [1]. Numerous ID groups in the country, including ours, have been able to address these challenges. This article aims to provide a framework for how success has been achieved through lessons learned, teamwork, diversification, and persistence.
Our Group
Metro Infectious Disease Consultants (MIDC) is a fully integrated ID group. After establishing the practice in suburban Chicago in 1994, MIDC has grown from 7 to over 125 ID physicians working in 8 states. We value mentorship, growth, collegiality, and educational stimulation. Over 3 decades, MIDC has navigated the somewhat turbulent landscape of healthcare, allowing physicians to attain a healthy work–life balance and, ultimately, to prosper.
Structure of the Group
To effectively facilitate decision-making and expedite management and financial processes within a group, a well-structured leadership framework is paramount. While multiple individuals may contribute to decision-making, a knowledgeable, identified leader is crucial. A single leader ensures consistency in contract negotiations, thereby enhancing opportunities for passive income. Key characteristics of such a leader include: the ability to comprehend interpersonal dynamics, a global financial perspective, the foresight to plan strategically, and the confidence to make challenging decisions. Another critical skill is the ability to identify ones own shortcomings. This can be supported by a medical management committee and the procurement of specialty non-medical skills, such as accounting services and legal counsel. Collegiality and the exchange of ideas are, of course, highly valued within a competitive group environment as they promote continual growth. It is essential, however, to have a single ultimate decision-maker to ensure consistency and accountability.
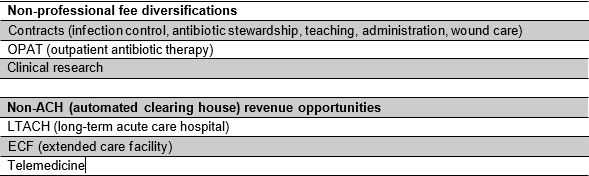
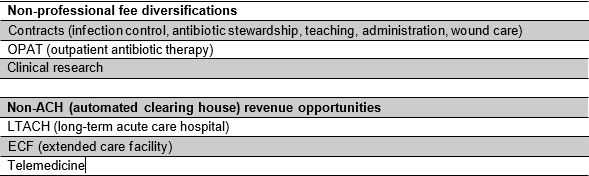
To take advantage of revenue diversification (Table 1), a group should be fully integrated and function under a single tax identification number. Groups in which each physician has a different number can limit the opportunities for growth as well as complicate the method by which costs are managed.
Achieving a work–life balance is paramount to every group. To achieve a reasonable balance, a group should ideally comprise at least 4 physicians, allowing for 1 weekend call per month. The inclusion of additional members would enhance the groups resilience during periods of sickness, unexpected emergencies, and fluctuating hospital volumes. Supporting inpatient management with physician extenders is a viable modality to decrease time spent on documentation and optimize time dedicated to actual patient care. This support is particularly valuable on weekends when time is limited. Outpatient support from office staff is frequently undervalued. Assigning a nurse to triage non-emergent calls from patients, extended care facilities, pharmacies, etc, spares the physician valuable time. When viewed through the lens of work–life balance, it is also cost-effective.
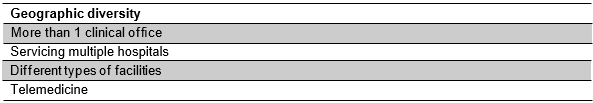
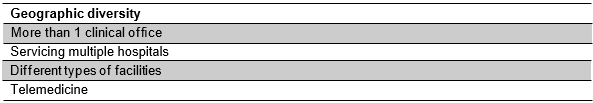
Geographic diversity (Table 2) provides enhanced financial security. In the current healthcare landscape, hospital systems are frequently acquired by other healthcare entities, such as private equity firms, leading to significant shifts in healthcare systems. These changes can impact an individual groups practice. Being credentialed at multiple hospitals offers greater flexibility in response to these shifts. Additionally, the environments surrounding different hospitals can change, with neighborhoods evolving, insurance payor mixes shifting, and, in some cases, hospitals closing due to financial unsustainability. Geographic diversity serves as a safeguard against the inevitable fluctuations within the American healthcare system.
Revenue Diversification
Revenue diversification provides financial flexibility and stability. These are critical when strategically planning for growth. Relying only on professional fee billing creates uncertainty, as a hospital census can vary depending on season, political environment, and hospital ownership. As ID physicians, we have an armamentarium of skills and abilities that allow for multiple sources of income, including contracts for infection control, antibiotic stewardship, and medical education. Other revenue opportunities require planning, space allocation, enhanced staffing, and procurement, and can include outpatient antibiotic therapy (OPAT), clinical research, travel medicine, telemedicine, and wound care. Telemedicine provides a unique opportunity for physicians who seek a more flexible lifestyle as well as opportunities to supplement their income.
All of these options are viable, but OPAT specifically provides not only a viable alternative revenue source, but also a seat at the healthcare reform table. Utilizing OPAT to streamline a transition to the outpatient arena, an ID consultant can influence length of stay as well as optimizing patient care [2]. While the operational details of an OPAT program are beyond the scope of this paper, we believe that this should be an anchor tenant of a private practice group.
In general, the more a group is able to incorporate revenue enhancements (Table 1) and diversification in their ID practice, the more stabilization will be realized.
Optimizing Productivity
Medical productivity can be defined as the ability to generate or enhance services. This may be realized in multiple fashions, such as volume of work performed, revenue generated, or opportunities afforded.
Having financial transparency allows leadership to gain trust while educating physicians on the business aspects of ID [3]. We achieve this by discussing with each individual physician their specific profit and loss statements. This allows for real-time feedback and gives the physician an opportunity to understand the specifics of cash flow and business development. Frequently discussed topics include the timeliness of billing, the value of interpersonal interactions, and the service orientation of a consultant. Ultimately, this should result in enhanced financial security.
Time management is critical to productivity as well as work–life balance, and in the realm of private practice, mastering the art of time management is essential. Mentoring new fellows on how to be efficient and productive is incredibly valuable [4,5]. It is likely that this will translate into a more organized and comfortable workforce, which will enhance future recruiting efforts.
Office Administration and Billing Infrastructure
To maintain a cost-efficient practice, optimal efficiency and productivity are essential for all staff members. Personal achievement directly correlates with financial rewards, effectively encouraging collaboration and productivity throughout the system.
Physicians, physician extenders, nurses, medical assistants, and the billing department are all financially incentivized. For example, our billing department receives a bonus based on submitted claims, motivating them to remind physicians to complete all billing tasks by 7 AM the following day.
Staffing ratios are difficult to ascertain, however, due to the multiple variables involved in the calculation. Nursing is key to the success of our practice. Each nurse brings a certain level of experience and training. For example, experienced nurses may feel more comfortable managing a higher number of infusions. Some medications require longer infusion times and complication risks. Smaller offices may have limited chair capacity. Patients with comorbidities may experience slower or interrupted treatment times due to complications. Attributes including individual nurses qualifications, characteristics of medications infused, the physical plant, and comorbidities with any anticipated complications, are all factored into the staffing equations.
Educational Infrastructure
Finally, cultivating an environment of camaraderie, academic collegiality, and academic stimulation generates stability and enhances personal fulfillment within a private practice group. Fifteen years ago, our group initiated the monthly Metro Educational Conference to present interesting cases and engage in discussions on management. This conference facilitated the exchange of innovative ideas, fostered a sense of fellowship, and nurtured collaborative relationships that promoted mutual support. During the pandemic, this concept evolved into a weekly Thursday educational conference, which was initially centered around real-time patient management for patients with COVID-19. Our physicians have uniformly contended that this conference was the most supportive and productive aspect of the pandemic and helped to bridge the educational gap presented by this disease. It has since evolved to encompass a review of ID concepts, point/counterpoint discussions, and challenging case presentations. In addition, our organization is accredited to provide category 1 CME to our providers. Participating in these educational activities ensures our groups competitiveness in an environment where possessing the most comprehensive knowledge helps to ensure the highest quality of care for our patients.
Conclusion
In summary, establishing a financially successful ID private practice necessitates strategic planning and thoughtful execution. Elements that are key to success include an effective leadership structure, revenue diversification, geographic diversity, optimized productivity and efficiency, and fostering an environment of education and collegiality. The provided outline serves as a guide, drawing upon the accumulated knowledge and experiences gained over 3 decades of practice by MIDC, a group that has successfully navigated the complexities of the healthcare industry.
Funding
This article received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Koval, M.L. Medscape Infectious Disease Physician Compensation Report 2024: Bigger Checks, Yet Many Doctors Still See an Underpaid Profession. 24 May 2024. Available online: https:// www.medscape.com/slideshow/2024-compensation-infectious-disease-6017140 (accessed on 26 March 2025).
- Petrak, R.M.; Skorodin, N.C.; Fliegelman, R.M.; Hines, D.W.; Chundi, V.V.; Harting, B.P. Value and clinical impact of an infectious disease-supervised outpatient parenteral antibiotic therapy program. Open Forum Infect. Dis. 2016, 3, ofw193. [CrossRef] [PubMed]
- Petrak, R.M.; Fliegelman, R.; Van Hise, N.W.; Chundi, V.; Didwania, V.; Han, A.; Harting, B. Private Practice Infectious Disease: Metro Infectious Disease Consultants. Priv. Pract. Infec. Dis. 2023, 3, 9. [CrossRef]
- Pitre, C.; Pettit, K.; Ladd, L.; Chisholm, C.; Welch, J.L. Physician Time Management. MedEdPORTAL 2018, 14, 10681. [CrossRef] [PubMed]
- This article summarizes key characteristics of a successful private practice group in Infectious Disease based on the experience of Metro Infectious Disease Consultants.Gordon, C.E.; Borka, S.C. Recapturing time: A practical approach to time management for physicians. Postgrad. Med. J. 2014, 90, 267–272. [CrossRef] [PubMed]

