
Abstract
A middle-aged man presented with sternal pain that progressed to the development of a sternal mass over the next few months. The subsequent workup and treatment are outlined, and the differential diagnosis is discussed.
Case Presentation
A 41-year-old man without chronic health problems presented to his primary care physician with mild to moderate sternal pain. He denied trauma, fever, weight loss, and night sweats. He also denied IV drug use and recent surgery. There was no record of his physical exam at that time, and he was told to take naproxen or acetaminophen to relieve his symptoms.
The pain gradually improved and seemed to resolve over the following 3 months. However, 8 months after the onset of symptoms, the sternal pain recurred. The patient continued to deny constitutional symptoms.
He went to his local emergency department (ED). He was afebrile; his white blood cell count was 6.3 K/μL, hemoglobin 15.1 g/dL, C-reactive protein (CRP) 1.1 mg/L, and Westergren sedimentation rate (ESR) was 27 mm/hr. Chemistries were normal.
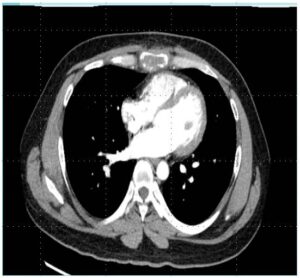
A computed tomography (CT) scan (Figure 1) was performed and showed a 4.1 cm lytic lesion within the sternal body with surrounding inflammation. No pulmonary infiltrates were noted.
A biopsy was recommended, and an outpatient consultation with a cardiothoracic surgeon was suggested; however, the patient never scheduled an appointment.
Three months after the ED visit, the sternal pain became more intense and the patient noted tender swelling over the lower part of his sternum. He still denied fever, but now was experiencing drenching night sweats.
He returned to his local ED and was found to have a large fluctuant mass over the lower sternum. He was afebrile, and his CBC and chemistry labs were normal.
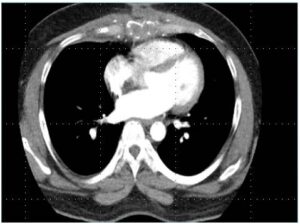
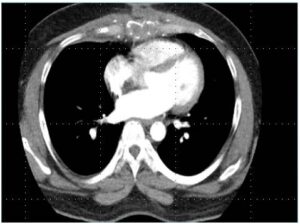
A repeat CT (Figure 2) was conducted and revealed a 13 ˆ 7 ˆ 7 cm soft tissue mass in the sternal body as well as enlarged mammary chain lymph nodes. No pulmonary lesions were noted.

The patient was admitted and underwent an ultrasound-guided needle biopsy. A total of 120 mL of purulent fluid was obtained. Gram stain did not reveal polymorphonuclear leukocytes or organisms. The patient was started empirically on piperacillin/tazobactam and vancomycin. Bacterial cultures remained negative and the patient’s pain improved.
The Infectious Diseases service was consulted 3 days after admission. They noted that the patient had no prior testing for mycobacterial infection despite being born in India and then arriving in the US 18 years earlier. There was no history of the patient having received bacillus Calmette-Guérin, and he denied intravenous drug use. Acid-fast bacillus (AFB) and fungal smears were requested on the purulent fluid that was aspirated; both were negative.
The patient was discharged on 4–drug therapy for tuberculosis (TB). Cytology was negative for malignancy.
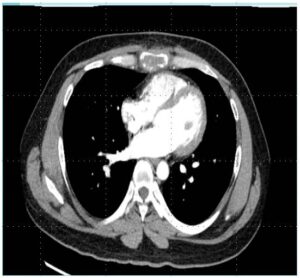
Over the next few weeks, drainage, pain, and swelling improved. A repeat CT 6 weeks into treatment (Figure 3) showed a marked reduction in the inflammatory mass. AFB cultures turned positive at 9 weeks, and 6 weeks later the AFB was identified as Mycobacterium tuberculosis susceptible to pyrazinamide.
Discussion
Most cases of sternal osteomyelitis are secondary to trauma and median sternotomy. Primary sternal osteomyelitis (PSO) is a rare disease, and its symptoms are often nonspecific, leading to a delay in diagnosis. It accounts for only 0.3% of bone infections and is usually a result of hematogenous seeding. Intravenous drug usage is a common risk factor [1].
The differential diagnosis of primary sternal osteomyelitis is very broad. While bacterial infections (especially Staphylococcus aureus) comprise the majority of reported cases, lytic sternal lesions may be due to almost any bacteria, as well as fungi and mycobacteria. In addition, noninfectious causes such as lymphoma, multiple myeloma, metastatic cancer, and sarcoid must also be considered [1].
PSO, as with our patient, typically presents with chest pain that eventually progresses to tenderness and swelling of the anterior chest. Spontaneous drainage and sinus tract formation may occur, as well as fever and chills. The diagnosis may be suggested by elevated levels of CRP and ESR, but these are nonspecific markers. Plain radiography has low sensitivity and specificity and may be normal early on. Nuclear medicine studies have very good sensitivity, but very poor specificity. Magnetic resonance imaging is probably the most sensitive noninvasive study; however, it may be more difficult to obtain than a CT scan. Likewise, FDG (18F-fluorodeoxyglucose) positron-emitting tomography/CT is very sensitive, but nonspecific, though it may be useful if there is suspicion of metastatic disease. CT is more available, has better bone resolution and is a reasonable initial study, especially in an ED or outpatient situation. However, none of these studies will differentiate which organism is causing the infection; therefore, tissue must be obtained and tested. While a bone biopsy is often not necessary when blood or aspirate cultures are positive, it should be strongly considered to look for malignancy, sarcoid, and granulomatous infections if routine cultures remain negative [1].
Even in endemic countries, sternal infection due to TB is rare, and is predominantly seen in middle-aged adults [2,3]. It arises primarily from hematogenous seeding, though it may also result from direct extension from hilar nodes or lymphatic spread. Potential complications of sternal TB include spontaneous fracture of the sternum, compression or erosion of the large blood vessels in the thorax, tracheal compression and spread to the mediastinum and pleural cavity [2,3]. Tubercular sternal osteomyelitis is treated similarly to other cases of extrapulmonary TB with 6–9 months of standard anti-tubercular therapy. Such therapy is usually sufficient in most patients, although surgical intervention may be necessary in the setting of an unstable sternum or lack of response to medical therapy [2,3]. Our patient continues to do well on TB therapy and has been able to avoid surgery.
Author Contributions
P.B. saw the patient and then shared the patients medical history; J.S. wrote the first draft and discussion. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
-
- Lopez, C.D.; Hill, J.B.; Stavropoulos, C.; Lerman, O.Z. Primary Sternal Osteomyelitis: A Case Report and Review. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2120. [CrossRef] [PubMed]
- Vasa, M.; Ohikhuare, C.; Brickner, L. Primary sternal tuberculosis osteomyelitis: A case report and discussion. Can. J. Infect. Dis. Med Microbiol. 2009, 20, e181–e184. [CrossRef] [PubMed]
- Sachdeva, R.; Sachdeva, S.; Arora, S. Sternal Tuberculosis. Ann. Med. Health Sci. Res. 2013, 3 (Suppl. 1), S21–S23. [CrossRef] [PubMed]

