HBV
CME credit can be obtained if questions are completed through the following link: https://www.eeds.com/em/3947
The following series of questions relates to HBV diagnosis and management.
25%
1 / 4
1. Which of the following is considered the main indicator of reactivation of previously resolved HBV (HBsAg-, anti-HBc+)?
Explanation : Answer: E. ALT rises to a much slower degree than HBV DNA and the formation of HBsAg and thus can not be used as an indicator of reactivated HBV. If one waits for an increase in ALT, reactivation has already begun.
 TABLE 1: Definitions of HBV Reaction Based on Society Guidelines
TABLE 1: Definitions of HBV Reaction Based on Society Guidelines
*CHB= Chronic Hepatitis B infection
Mynt A, et al. Clin Liver Disease, Vol 15, No 4, April 2020
 TABLE 1: Definitions of HBV Reaction Based on Society Guidelines
TABLE 1: Definitions of HBV Reaction Based on Society Guidelines
| Baseline Serologies | HBsAg+, anti-HBc+ | HBsAg-, anti-HBc+ |
| AASLD 2018 | Unknown DNA baseline: >10k IU/mL Known DNA baseline, previously undetectable: >1000 IU/mL Known DNA baseline, previously detectable: >100-fold increase | Development of detectable DNA or development of HBsAg (AKA reverse seroconversion) |
| AGA 2015 | Unknown DNA baseline: not explicitly defined Known DNA baseline, previously undetectable: de novo detectable DNA Known DNA baseline, previously detectable: >10-fold increase | Development of detectable DNA or development of HBsAg or development of HBeAg |
| APASL 2016 | Unknown DNA baseline: >20k IU/mL Known DNA baseline, previously undetectable: >100 IU/mL Known DNA baseline, previously detectable: >100-fold increase | Development of detectable DNA or development of HBsAg |
| EASL 2017 | Not explicitly defined | Not explicitly defined |
50%
2 / 4
2. You are asked to evaluate a patient with a history of Hepatitis B virus who is scheduled to receive Rituximab for Non Hodgkin’s lymphoma (NHL). He arrives with a set of blood work from his oncologist’s office. Results demonstrate HBsAg+ and HBcAb+ with an undetectable HBV DNA. What do you recommend to his oncologist regarding HBV prophylaxis?
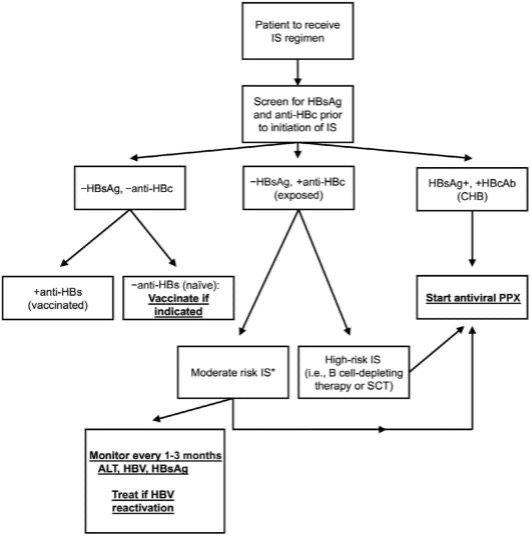
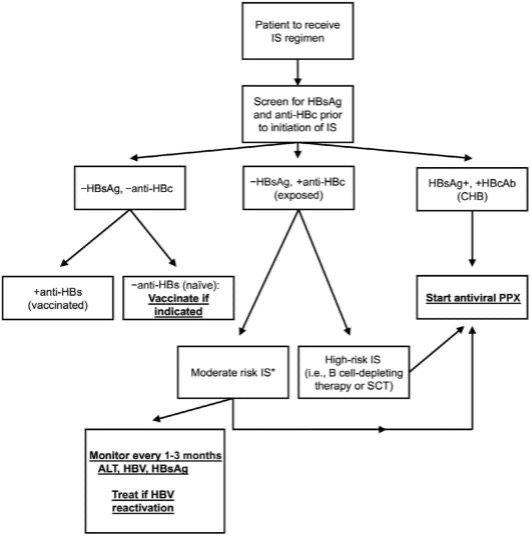
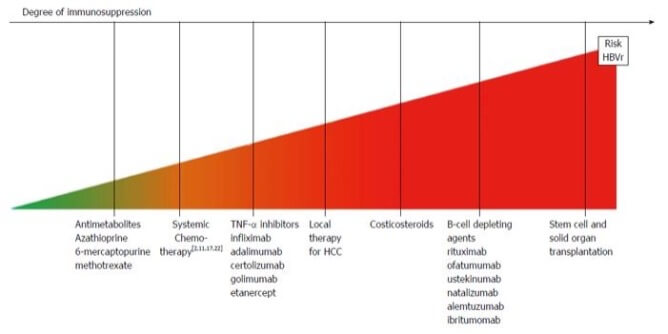
Explanation : Answer: D. Any patient that has chronic hepatitis B (HBsAg+, HBcAb+) regardless of detectable DNA is at risk for reactivation, regardless of immunosuppression planned and should receive antiviral prophylaxis. This should always be continued after the immunosuppressive agent has been discontinued. Duration of therapy ranges from 6-12m after cessation for moderate immunosuppressive agents; 12-18m for high risk agents (B cell depleting agents/anti-CD20 or SCT). Rituximab is considered a high immunosuppressive agent.
* Please see flowchart listed after question 3.
75%
3 / 4
3. Another patient with a PMH of Crohn’s Disease that is about to be started on Adalimumab (Humira) arrives to you because her gastroenterologist is concerned about the potential of HBV reactivation given her history of the infection in the 1990’s. Her baseline labs include the following: HBsAg-, HBc Ab+ and undetectable DNA. What do you recommend for prophylaxis?
Explanation : Answer: E. Either A or C is acceptable. The patient has resolved Hep B with undetectable DNA which makes her moderate risk for reactivation. The use of TNF-alpha agents (including adalimumab), cytokine inhibitors, integrin inhibitors, and low dose corticosteroids are also considered to have a moderative risk of immunosuppression. Most societies would recommend serial labs but prophylaxis can be considered especially in patients that may not be reliable to follow up.
*Please see the following flowchart and table.
 Mynt A, et al. Clin Liver Disease, Vol 15, No 4, April 2020
Mynt A, et al. Clin Liver Disease, Vol 15, No 4, April 2020
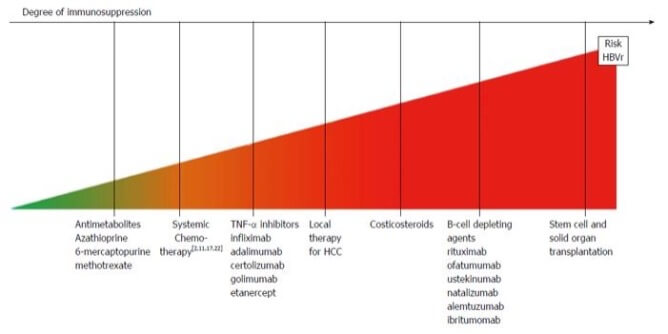 Bassone F, et al. World J Hepatol. Mar 18, 2016; 8(8): 385-394
Bassone F, et al. World J Hepatol. Mar 18, 2016; 8(8): 385-394
 Mynt A, et al. Clin Liver Disease, Vol 15, No 4, April 2020
Mynt A, et al. Clin Liver Disease, Vol 15, No 4, April 2020
 Bassone F, et al. World J Hepatol. Mar 18, 2016; 8(8): 385-394
Bassone F, et al. World J Hepatol. Mar 18, 2016; 8(8): 385-394 100%
4 / 4
4. Which of the following anti-viral agents would you recommend for HBV prophylaxis?
Explanation : Answer: E. Answers A, B and C
Both tenofovir formulations and entecavir are considered 1st line therapy for HBV prophylaxis. They both have shown lower rates of reactivation and barriers to resistance compared to lamivudine.
(Yang et, al. Ann Hepatol 2016: 15: 501-511; Picardi, et al. Blood 2019: 133:498-501.)
Thank you for completing the questions!
There were a total of {{total_questions}} questions of which you answered {{correct_count}} question(s) correctly and {{wrong_count}} question(s) incorrectly.

